Low-Dose THC Has Positive Effect on Morbidity, Quality of Life and Mortality in Geriatric and Palliative Patients
Posted: October 22, 2022 Filed under: Food and it's Impact on Our Health, Non-Toxic Choices | Tags: #meals #vegetarian #glutenfree #delivery #Jacksonville #nutrioncoaching #lactosefree #weightloss #immunesystem Leave a commentThe study was published by the peer-reviewed journal peer-reviewed journal MMW – Fortschritte der Medizin, as well as on the website for the U.S. National Library of Medicine.
“Cannabis-containing medicines have been successfully used in our practice for more than 20 years in pain and especially in geriatric and palliative patients”, notes the abstract of the study. “While it was initially a very indication-specific use (pain, loss of appetite, etc.) and also with higher THC doses, this changed over time to low THC doses and a therapy focus on suffering-perpetuating symptoms and especially on stress (Matrix of Symptoms).”
As part of the legally prescribed companion survey, researchers “evaluated our data in parallel and discussed it publicly in a series of publications. Based on these published results, the article is intended to show an overview of our experiences.”
Researchers found that “Low-dose THC has a positive effect on morbidity, side effects, quality of life and mortality in geriatric and palliative patients.”
They conclude by stating that “Early therapy is particularly appropriate in geriatric and palliative patients due to the clear benefit-risk ratio of low-dose THC.”
Below is the study’s full abstract.
Abstract
Background: Cannabis-containing medicines have been successfully used in our practice for more than 20 years in pain and especially in geriatric and palliative patients. While it was initially a very indication-specific use (pain, loss of appetite, etc.) and also with higher THC doses, this changed over time to low THC doses and a therapy focus on suffering-perpetuating symptoms and especially on stress (Matrix of Symptoms).
Method: As part of the legally prescribed companion survey, we evaluated our data in parallel and discussed it publicly in a series of publications. Based on these published results, the article is intended to show an overview of our experiences.
Results: Low-dose THC has a positive effect on morbidity, side effects, quality of life and mortality in geriatric and palliative patients.
Conclusion: Early therapy is particularly appropriate in geriatric and palliative patients due to the clear benefit-risk ratio of low-dose THC.
My Level of Living Green
Posted: October 19, 2022 Filed under: Going Green; How and Why..., Non-Toxic Choices | Tags: #meals #vegetarian #glutenfree #delivery #Jacksonville #nutrioncoaching #lactosefree #weightloss #immunesystem Leave a commentI started my Blog in 2008, I woke up one morning and had gotten 5000 visits from all over the world! No Impact M<an had seen my site and published the article that put my Blog on the map!!
Here is that article…
I am soooo excited! One of my all time favorite bloggers, Colin Beavan, published an article from my blog! His blog, NoImpactMan.com, is a blog that I follow religiously. I have always been a a serious environmentalist, way before it was cool the first time around..and I am talking back in 1972 when I decided to use cloth diapers instead of that new product (Pampers) everyone else was sooo excited about. I still chose to use a clothesline with the first 4 kids diapers (until I moved to a neighborhood (yuck!) that forbid clotheslines.
Colin’s’ blog made me realize there was a LOT more I could be doing. Hence, the list he published….
April 14, 2009
Thirty-one tips for reducing your impact while saving money
I was reading through comments here on the blog last night and I found this great list of tips by reader Millie Barnes, who writes a blog about health and gardening called Optimum Nutrition. Her tips were just too comprehensive to let them languish in the comments. So here they are (I don’t even mind including the plug for her products). Thanks Millie!
My Level of Living Green
by Millie Barnes
1) Air dry all laundry–had to put a lock on the dryer cord to convince my daughters I was serious–they have learned to plan ahead! I wash all laundry in cold water, always wash full loads, and use a drying rack inside if it is raining. It’s good for the earth and great for your skin, a free humidifier in the house. Which also makes it feel a few degrees warmer in winter, and cooler in summer. I use soapnuts for laundry. http://www.zamuta.com/
2) Buy all organic.
3) Buy all organic non-toxic beauty care products and make-up. I make my own skin care cleanser and moisturizers. I make my own soap.
4) Use baking soda and vinegar for cleaning the bathroom. I use Ms. Meyer Clean Day for dishes, Citri-Clean for counters and general purpose cleaning. I use a loofah for scrubbing dishes (I am growing my own right now so I won’t have to buy them anymore!) My sister is making scrubbies by crocheting them, we will offer these for sale soon!
5) Take cloth bags to store for groceries and all other purchases. Take muslin bags I made to grocery store for produce.
6) Recycle, re-use, make my own and have stopped buying anything I don’t really need.
7) Don’t use paper towels, never have. Used cloth diapers for all 5 kids.
8) Don’t buy stuff in plastic, I try to buy all glass. Store all food in glass. Re-use glass jars. I mostly buy real food (meat, produce) try to not buy anything that needs a label, so no packaging.
9) I use a bidet and cloth wipes. (don’t freak, we all used that same choice when we used cloth diapers and wash clothes on our baby’s tushes!)
10) Make my own gluten free granola, make my own mayonnaise, salad dressings, spice blends.
11) I use a compost toilet, no toilet paper (think cloth baby wash clothes).
13) Bokashi (a way to deal with indoor kitchen scraps with NO odor and yields compost WAY faster). I have been using the Bokashi method of dealing with kitchen waste for about 3 weeks now…I love it!
14) Use very low flow shower heads. Ace Hardware has a 1.5 GPM with a shut-off valve.
15) Use all CF light bulbs…and use them as little as possible. I have one evening a week that I use no lights..on Shabbat! Dinner by candlelight!
16) Use grey water from shower (I keep a 3 gallon bucket in shower and use it throughout the day to flush the toilet, take what’s left to the flower beds.
17) Use water from rinsing dishes to water flower beds.
18) Run as few errands as possible, car pool and combine trips.
19) Use micro-cloths to clean with, even on glass you do not need cleaning products!
20) NEVER buy bottled water. I bought a Kleen Kanteen for each person in the family, we refill and take with us. I’ve had mine over a year.
21) Go paperless or CD-less as much as possible. I provide my clients with emails of my book, but still put cookbook software on CD.
22) Use only a hurricane lamp when we sit outside at night. It gives enough light to read by…but is perfect turned low …for just hanging out. Very romantic, too!
23) Use candlelight at dinner, not just on Shabbat!
26) I put in a raised bed garden, square foot garden I have green leaf lettuce in a grow box, cherry and big sweet tomatoes, basil, thyme. I have sweet potatoes growing, beets (mmmm, beet greens), onions, Swiss chard, purple flowering kale, nasturtiums, broccoli, cucumbers, peppers, red potatoes, a banana tree. Inside I am growing cucumbers and strawberries hydroponically.
27) I use a non-disposable razor, an old-fashioned stainless steel, very high quality razor that uses double edged blades. It was 24.00 from ClassicShaving.com. The blades are 10 for 5.99, and they are double edged! They give the closest, smoothest shave you can imagine! No disposable blade can compare.
28) Wash dishes with 2 dish pans in the sink, one for hot soapy water, one with warm rinse water. Do glasses first, pause a moment to let the soapy water drip off, then move to rinse water. Stop when rinse water is almost full and rinse quickly. Repeat with silver, plates, then pots and utensils. All with 2 dishpans full of water. Then I pour the soapy water, with all that organic matter, onto my plants in the garden. It helps repel pests and loosens the soil. And good for the biceps when you carry it outdoors.
29) I water my garden with buckets from the rain barrels that are under the eaves of my garage. 10 feet from my garden. The front flower garden gets watered entirely from the dish water.
30) I work out at home, no expensive gym memberships that I never used anyway. I save all the expense of membership, and gas and time driving. I have a set of weights, two exercise balls, a yoga mat and a chin-up bar.
Lipophilic Statin use Linked to Increased Risk of Dementia
Posted: August 2, 2021 Filed under: Food and it's Impact on Our Health, Non-Toxic Choices | Tags: #allergies, #BeyondPaleo, #cancer, #energy, #energy #pontevedrabeach, #glutenfree, #healing, #higherenergy, #immunesystem, #JacksonvilleFL, #jax, #Lactosefree, #mealdeliveryservice, #nutritioncoaching, #plantbased, #weightloss Leave a commentReston, VA (Embargoed until 7:30 p.m. EDT, Monday, June 14, 2021)–In patients with mild cognitive impairment, taking lipophilic statins more than doubles their risk of developing dementia compared to those who do not take statins. According to research presented at the Society of Nuclear Medicine and Molecular Imaging 2021 Annual Meeting, positron emission tomography (PET) scans of lipophilic statin users revealed a highly significant decline in metabolism in the area of the brain that is first impacted by Alzheimer’s disease.
Statins are medications used to lower cholesterol and reduce the risk of heart attack or stroke. They are the most commonly used drugs in the developed world, and nearly 50 percent of Americans over age 75 use a statin. Different types of statins are available based on a patient’s health needs, including hydrophilic statins that focus on the liver and lipophilic statins that are distributed to tissues throughout the body.
“There have been many conflicting studies on the effects of statin drugs on cognition,” said Prasanna Padmanabham, project head, statins and cognition in the molecular and medical pharmacology student research program at the University of California, Los Angeles in Los Angeles, California. “While some claim that satins protect users against dementia, others assert that they accelerate the development of dementia. Our study aimed to clarify the relationship between statin use and subject’s long-term cognitive trajectory.”
Researchers separated study participants into groups based on three parameters: baseline cognitive status, baseline cholesterol levels and type of statin used. Participants underwent 18F-FDG PET imaging to identify any regions of declining cerebral metabolism within each statin group. Eight years of subject clinical data was analyzed.
Patients with mild cognitive impairment or normal cognition who used lipophilic statins were found to have more than double the risk of developing dementia compared to statin non-users. Over time, PET imaging of lipophilic statin users also showed a substantial decline in metabolism in the posterior cingulate cortex, the region of the brain known to decline the most significantly in the earliest stages of Alzheimer’s disease. In contrast, no clinical or metabolic decline was found for users of other statins or for statin users with higher baseline serum cholesterol levels.
“By characterizing the metabolic effects associated with statin use, we are providing a new application of PET to further our understanding of the relationship between one of the most commonly used classes of drugs and one of the most common afflictions of the aging brain,” noted Padmanabham. “Findings from these scans could be used to inform patients’ decisions regarding which statin would be most optimal to use with respect to preservation of their cognition and ability to function independently.”
About the Society of Nuclear Medicine and Molecular Imaging
The Society of Nuclear Medicine and Molecular Imaging (SNMMI) is an international scientific and medical organization dedicated to advancing nuclear medicine and molecular imaging, vital elements of precision medicine that allow diagnosis and treatment to be tailored to individual patients in order to achieve the best possible outcomes.
SNMMI’s members set the standard for molecular imaging and nuclear medicine practice by creating guidelines, sharing information through journals and meetings and leading advocacy on key issues that affect molecular imaging and therapy research and practice. For more information, visit http://www.snmmi.org
JOURNAL
GIR Reusable Face Masks- the only mask I wear anymore!
Posted: January 3, 2021 Filed under: Health and Happiness, Non-Toxic Choices, Products Leave a commentMy GIR mask is now the only one I wear! They run a tad small and I ordered a medium, which fits me perfectly. BUT they run small!
All of you who follow my blog know that I very rarely endorse products. However I have to share this! We are 11 months in to the pandemic and I now have a fabulous collection of masks. But wearing glasses with them is tricky and so is he fact that every single mask has to be modified because my face and especially my nose is SO tiny. I wear children’s glasses and my nose width at the tip of my nose is only 1/2 an inch wide. I have long been a fan of GIR kitchen utensils. As a Chef and an environmentalist I do not use plastic and love the well designed silicone utensils.
And then when the epidemic started they added a mask to their repertoire. HOLY COW, it is perfect! The silicone seals the mask around my face, the ear straps are perfect and the cleaning is a cinch. Just wash with soap and hot water and you are set to go. All of my cloth masks are wearing out at this point, this solves that problem. My glasses do not fog up because no moist are is escaping EXCEPT through the vent in the front of the mask. That means I am breathing in and out completely filtered air!
The filters are great but are pricy, so I use my own charcoal masks with 2 non-woven paper filters.
What Can We Do To Reduce Waste?
Posted: November 12, 2020 Filed under: Food and it's Impact on Our Health, In The Kitchen with Millie- How To's, Non-Toxic Choices | Tags: #allergies, #atlanticbeach, #BeyondPaleo, #cancer, #energy, #energy #pontevedrabeach, #glutenfree, #healing, #higherenergy, #immunesystem, #JacksonvilleFL, #jax, #Lactosefree, #mealdeliveryservice, #nutritioncoaching, #weightloss Leave a commentNovember 10, 2020
In our series “Simple Steps to Sustainability,” experts from around the world give us their tips and tricks on how to live more sustainably.
Sustainable living is hard enough, now add the pressures of a global pandemic and all bets are off.
So we tracked down some experts and asked: What can we do to reduce waste?
“The single biggest source of waste that goes to municipal landfills is wasted food,” Peter Wright, the Assistant Administrator of the EPA’s Office of Land and Emergency Management, told Newsy.
“If food waste was a country, it would be the third biggest polluter after the U.S. and China,” Lucie Basch, the co-founder of Too Good To Go, said. “It’s 50% of people who don’t even know that there are several dates. The ‘best before’, for example, means that the quality is going to be perfect until that date. But it doesn’t mean after that date you can’t eat the product anymore.”
“To reduce your waste, you want to start looking at refusing taking things you’re going to have to throw away in the first place,” Alexander Furey, the founder of Zero Waste Mindset, said.
“Stock up on maybe some pantry staples in such a way that rather than getting a bunch of small bags of things wrapped in plastic, you could get one thing that you then divide up among your community,” Jocelyn Quarrell, the CEO and owner of Go Box, said.
“Maybe doing a waste audit of your home,” Furey said. “And every time you put something in the black bin, in the rubbish bin, write down what you put in. And then after a week, go back and look at your list and see if you can see patterns of the kinds of things you’re throwing away.”
For more videos on how to live sustainably, visit newsy.com/sustainability.
Is Dimethicone in Natural Skincare Products Good or Bad for Your Skin?
Posted: July 9, 2020 Filed under: Non-Toxic Choices, Skin Care | Tags: #allergies, #atlanticbeach, #BeyondPaleo, #cancer, #energy, #energy #pontevedrabeach, #glutenfree, #healing, #higherenergy, #immunesystem, #JacksonvilleFL, #jax, #Lactosefree, #mealdeliveryservice, #nutritioncoaching, #weightloss Leave a commentMillie- Even though I have always used organic or natural skin and makeup choices I have been alarmed at how many so-called natural and organic products contain silicones. Another chemical that most organic products have is Butylene glycol. It is a petroleum product that hey consider organic. The word organic means nothing more than “ noting or pertaining to a class of chemical compounds that formerly comprised only those existing in or derived from plants or animals, but that now includes all other compounds of carbon”. It has been tough finding effective skin products without these items. While I can tolerate silicones with no reaction, I do find that using products with them makes my serums and moisturizers less effective. The reason for this is that silicones sit on top of the skin and form a barrier, so that treatments aren’t effective as they do not reach the skin. So my oils and moisturizers cannot nourish the skin. Also it does not let the skin breath properly. I have spent a year experimenting with my skin care, and my skin looks far better with products that are not occlusive to his degree.
Have you ever wondered what makes your favourite moisturizer light as air and non-greasy? It’s simple: you can thank silicone for that kind of texture.
Yes, silicone – the umbrella term for a countless number of synthetic polymers whose place in clean beauty has been called into question on more than one occasion. However, silicones aren’t new to the industry.
First introduced in the ’50s, cosmetic grade synthesized silicon-carbon polymers (also known as silicones) offered companies a number of characteristics that made improving the feel, appearance, and performance of cosmetic products infinitely better.
Today, silicone compounds are being developed in many different shapes and forms, from fluids to powders. In natural products, like sunscreen, an emollient called dimethicone gives life to some of the most luxurious, desirable textures on the market.
The downside? Like any other synthetic ingredient, there have been negative effects associated with prolonged use of dimethicone on the skin. The verdict on this ingredient amongst industry professionals is truly a mixed bag, which makes forming an opinion about whether or not its a “good” or “bad” substance a bigger challenge.Though some might suggest avoiding silicones like dimethicone at all costs, it may not be necessary.
Here, you’ll discover all you need to know about dimethicone and its benefits. Plus, Sara A. Dudley, CEO of The Sunscreen Company, weighs in on dimethicone in sun care products.
What is dimethicone?
By definition, silicone is a synthetic polymer made up of silicon, oxygen, and other elements like carbon and hydrogen. Dimethicone works well with humectants – agents that help retain the skin’s moisture levels.
Found prominently in creams, lotions and primers for its ability to moisturize the skin without feeling heavy, dimethicone is frequently used as a substitute for petrolatum-based ingredients.
The silky, spreadable texture of dimethicone allows products to be applied smoothly and fills in wrinkles and fine lines, resulting in an even appearance. These properties often produce an effect that makes you think a product is “working” despite the fact that its effects are temporary.
Why use it?
Back in 2017, founder and editor of The Skincare Edit, Michelle Villett, summed up the reasons why silicones like dimethicone are used by brands in the most concise way: they’re smoothing, water resistant, and they’re inexpensive for companies to purchase and include in their formulas.
The pros
Aside from moisturizing and smoothing skin without feeling heavy, dimethicone can also be used to treat sensitive skin.
“It can actually help people with compromised skin barriers because it’s occlusive. For my infant son, for example, we use a body moisturizer that has a little dimethicone in it for his eczema because he needs the added protection,” said Dudley.
Although Dudley views the dimethicone “grey zone” in clean beauty as an interesting topic, she doesn’t believe the product is actually harmful to the skin.
“It has been overused in a lot of conventional products because it tricks consumers into thinking it’s giving extra hydration. It will make skin or hair look good in the short term but it’s not really treating or hydrating the skin in a beneficial way,” she explained. “From a sunscreen standpoint, it can help with spreadability, especially for mineral sunscreens that have really large particulates in them.”
The cons
A long-standing debate persists about whether or not silicones like dimethicone cause clogged pores, irritation and prevent other ingredients from absorbing into the skin. However, it’s been said that there’s no scientific basis for those claims, since silicones are “pure synthetics” specially formulated to avoid clogging pores and irritating the skin.
Another reason why dimethicone is viewed negatively is because of its occlusive nature, which forms a barrier on the skin that’s been said to “exacerbate acne” by trapping moisture, bacteria, sebum, and other impurities.
Dudley notes consumers concern about the bioaccumulation of particles from silicones in water systems, and for this reason, The Sunscreen Company has removed it from their products.
“I think it gets a bad rap as being not natural, although I would argue it’s just further down the chain of what is considered naturally derived,” said Dudley. “It’s considered a cheap ingredient or filler, something designed by big brands to dupe customers. I think it can have a place in clean beauty, but it just needs to be used a lot more judiciously and transparently than what has been done in the past.”
Your verdict:
After weighing both sides of the case on dimethicone, it turns out that your judgement is the most important factor in deeming how safe or unsafe it is to use on the skin.
To learn more about the potentially adverse affects on the body and the environment related to dimethicone, EWG’s Skin Deep is a great resource. The scientific findings about dimethicone’s “harmfulness” are limited, though its been proven time and time again to serve as a less toxic alternative to pesticide-containing products.
#mealdeliveryservice, #jax,#lactosefree,#glutenfree,#JacksonvilleFL,#nutritioncoaching, #allergies,#cancer,#energy,#higherenergy,#healing, #beyondpaleo, #immunesystem, #weightloss, #energy #pontevedrabeach, #atlanticbeach
Study: Drinking dairy milk linked to breast cancer in women
Posted: March 1, 2020 Filed under: Food and it's Impact on Our Health, Non-Toxic Choices Leave a commentNote from Millie– Dairy foods do not belong in the human body. Breastfed until 2 years old and after that we do not need dairy.
New U.S. research has found that drinking even a moderate amount of dairy milk appears to be linked to an increased risk of breast cancer in women.
Hot on the heels of a review from top nutrition scientists that cautioned against drinking cow’s milk comes another study with another caution: drinking milk increases the risk of developing breast cancer, say the researchers. But this finding comes from an observational study, and there may be confounders that are not accounted for, says an expert not involved with the study.
The latest research was based on data from the long-running larger study called Adventist Health Study-2 (AHS-2), which is looking at diet and health among Seventh Day Adventists in North America. Past results from this study have suggested that Seventh Day Adventists have longer life spans and lower rates of some cancers, perhaps because of heathier lifestyles.
The latest analysis suggests that milk raises breast cancer risk, and the more you drink the higher your risk may be.
“Consuming as little as 1/4 to 1/3 cup of dairy milk per day was associated with an increased risk of breast cancer of 30%,” first author Gary E. Fraser, MBChB, PhD, said in a press statement. Fraser is affiliated with the School of Public Health at Loma Linda University, California.
“By drinking up to 1 cup per day, the associated risk went up to 50%, and for those drinking 2 to 3 cups per day, the risk increased further to 70% to 80%,” he added.
The findings were published February 25 in the International Journal of Epidemiology.
“The AHS study is provocative, but it’s not enough to warrant a change in guidelines. The caution being espoused by the authors is not warranted given the observational nature of this study,” commented Don Dizon, MD, director of Women’s Cancers, Lifespan Cancer Institute at Brown University in Providence, Rhode Island. He was not involved with the study and was approached by Medscape Medical News for comment.
Because of its observational design, the study cannot prove that cow’s milk causes breast cancer, Dizon emphasized.
“I’d want to see if the findings are replicated [by others]. Outside of a randomized trial of [cow’s] milk vs no milk or even soy, and incident breast cancers, there will never be undisputable data,” he said.
“Probably the biggest point [about this study] is not to overinflate the data,” Dizon added.
He noted that the results were significant only for postmenopausal women, and not for premenopausal women. Moreover, analyses showed significant associations only for hormone receptor-positive cancers.
Is Clean Beauty Really Better? 7 Derms & Aestheticians Weigh In
Posted: October 25, 2019 Filed under: Non-Toxic Choices, Skin Care Leave a commentThese doctors have voiced how important clean skin care is, but the recommendations they make (about thoer own skincare lines) are WAY OFF BASE! Many of these products include toxic ingredients such as butylene glycol, Sodium Hyaluronate, Glycerin, etc. Even products labeled natural or even organic contains these 3 ingredients which wreak havoc on the skin. Every skincare product they recommend (which they sell) are devoid of toxic ingredients. The last one list doesn’t give an igredient list on their pages that sell the product!
Scan almost any clean beauty retailer’s “About” page — Detox Market, Credo, Follain, Beautycounter — and you’ll notice two keywords: health and safety. That’s because the movement’s overarching mission is to eliminate chemicals ,known to be toxic to the human body from personal care products, including suspected cancer-causing agents (formaldehyde releasers, parabens) and hormone disruptors (phthalates, pesticides). While that’s no doubt a win for overall wellness, it does leave one critical question unanswered: Is clean beauty better for your skin? These seven dermatologists, cosmetic chemists, and renowned aestheticians think so.
“From my unique vantage point as a facialist for the past 25 years, having treated over 25,000 faces, I have seen how the proliferation of harsh ingredients — including dimethicone, fragrance, colorants, and sulfates — compromise the skin’s lipid barrier, thereby sensitizing the skin,” Angela Caglia, a celebrity aesthetician who works with Barbra Streisand and Minnie Driver, tells The Zoe Report. The integrity of the skin barrier is also a sticking point for cosmetic scientist Dr. Shuting Hu, Ph.D., who works with clean beauty brand Acaderma. “I personally believe in using clean ingredients as it is the very best way to prevent skin irritation and skin barrier damages, both of which are better for skin health,” Dr. Hu tells TZR. “Not only is it my belief, it is also scientifically proven.”
There’s a catch, though: Terms like “clean,” “natural,” “green,” and “non-toxic” aren’t regulated by the FDA — so, in theory, any brand can market any ingredient as clean (although the threat of callout culture tends to keep companies in line). “We really need a good working definition for ‘clean’ and ‘non-toxic,’” Marie Veronique Nadeau, a chemist and founder of her namesake skincare line, tells The Zoe Report. She personally considers an ingredient clean when it has “a track record for safety and efficacy” via scientific studies — and that goes for both naturals and synthetics. “It just makes more sense to use ingredients that are safe in your own opinion,” she says.
Ahead, seven skincare experts explain why they believe clean beauty is the healthiest choice for your skin — and reveal the natural and non-toxic products they swear by.
Dr. Nava Greenfield, Board-Certified Dermatologist
You need to be just as careful about what you put on your skin as what you eat and drink,” Dr. Nava Greenfield, M.D., a board-certified dermatologist, tells TZR. “Numerous studies have confirmed that products used topically on the skin penetrate into the bloodstream and affect your body.” She suggests cross-checking your products with the Environmental Working Group’s toxicity database to pinpoint any potentially harmful ingredients.
Marie Veronique Nadeau, Chemist & Brand Founder
“Absolutely, ‘clean’ and ‘non-toxic’ ingredients are better for the health of the skin,” Nadeau says. When it comes to formulating her own products, Nadeau adds a third descriptor to the list: active. “It’s not enough that it won’t harm you — people also need to be asking, ‘Is it active? Is it going to be doing something for my skin?’”
To this end, she recommends incorporating clean versions of vitamin C and vitamin B3 — aka, niacinamide — into your routine. “You need vitamin C to build collagen, and it also does any number of other cool things like limit hyperpigmentation and provide UV protection,” Nadeau says. “Vitamin B3 protects mitochondrial DNA from free radical damage. This is about as close as we’re going to get to slowing the aging process in the skin, so it’s a must-have for anyone interested in keeping skin healthy and youthful-looking.”
Britta Plug, Aesthetician & Brand Founder
“I avoid processed food and chemicals — I feel my best that way — and I apply the same reasoning to my skincare,” Britta Plug, a holistic aesthetician and co-founder of Wildling, tells The Zoe Report. According to Plug (and science), harsh chemicals can negatively impact the skin’s microbiome and disrupt its inherent functions. “Natural products are much more likely to support the skin’s innate intelligence, and support all of its functions, flora, and barrier system,” she says.
Her go-to products, naturally, come from her own line. “I’m obsessed with the sweet fern in our Empress Tonic,” Plug says. “It’s amazing for kickstarting detoxification by stimulating lymphatic flow, and it’s also great for skin irritations.” After spritzing with the Tonic, she reaches for Wildling’s Empress Oil. “The balm of gilead in the oil is pure magic for stimulating circulation and reducing fine lines and breakouts,” the aesthetician explains. “It also smells like a dreamy forest.”
Dr. Shuting Hu, Cosmetic Scientist
Dr. Hu is passionate about clean skincare — but emphasizes that clean doesn’t always mean natural. “Plenty of natural ingredients are irritating, and not all natural materials are made equally,” she says. “Some high quality synthesized ingredients are also clean, like vitamin C.”
In her work with Acaderma, Dr. Hu defines “clean” as any ingredient that minimizes irritation to the skin while maintaining efficacy. Her favorite? “Seh-Haw EXTM,” a brand-exclusive form of African kinkeliba extract that moisturizes dehydrated skin and boosts the barrier. “We spent two years optimizing the extraction and purification process of Seh-Haw EXTM to make sure no organic solvents were used in the whole process, and that there were no causes of pollution to the environment,” she says.
Angela Caglia, Celebrity Aesthetician & Brand Founder
“Through a process of trial and error in my treatment room, I’ve discovered which ingredients work and which ingredients make skin more susceptible to external aging factors,” Caglia says. (Considering her clients include age-defying celebs like Helena Christensen, I totally trust her.)
“One ingredient, in particular, that I’ve discovered helps with maintaining homeostasis is the organically-grown Limnanthes alba flower, indigenous to the Pacific Northwest, from which meadowfoam seed oil is derived through a unique cold pressing process,” she shares. “The reason why I love it is that it’s similar in molecular structure to our own sebum, which means it’s able to deeply penetrate the skin’s surface to deliver high levels of essential fatty acids and antioxidants where they’re needed most.” It can be found throughout the aesthetician’s namesake skincare line.
Athena Hewett, Aesthetician & Brand Founder
“Like much of the population, I have sensitive skin,” Athena Hewett, an aesthetician and founder of skincare brand Monastery, tells The Zoe Report. When she discovered that even hypoallergenic ingredients were irritating her skin, she decided to launch her own company — where she’s redefined “non-toxic” as “100 percent natural.”
“Take propylene glycol, for example — this chemical is used to make polyester, is considered non-toxic, and is found in nearly all of the skincare products out today,” she says. “I am highly allergic to this ingredient as are many of my clients, but most of them have no idea that this is what has been wrong with their skin. When someone lays on my table and I notice dermatitis, I can almost guarantee that they are putting propylene glycol on their skin in some form or another. Sadly, this ingredient is just one of many.” Hewett now looks to naturals for safe — and sensitivity-friendly — skincare solutions. “I love watching what raspberry seed oil does to the skin,” she says. “It makes up our Gold Oil, and it immediately soothes and reduces redness.”
Sarah Akram, Aesthetician
“I am a believer in integrative skincare, meaning just like what you put inside of your body, what you put on its surface can make a big difference in how you look and feel,” Sarah Akram, a Washington D.C.-based aesthetician and the founder of her namesake skincare boutique, tells TZR. “Just like you’d drink a cold pressed juice for optimum nutrient intake, you should take a similar approach to your skincare routine and overall skin health.”
She suggests looking for products packed with pure, natural ingredients (i.e., not “naturally-derived” — which is basically a synonym for “synthetic”). The facialists’ top pick? The Antioxidant Defence Creme by Environ. “This moisturizer is loaded with antioxidants like vitamin C and E to strengthen skin cells and fight free radicals,” Akram says. “Antioxidants are so important in the fight against premature aging, they actually work with your SPF to protect and correct the effects of harmful UV rays.” And, of course, they’re abundant in nature.
Artificial Leaf Turns Sunlight, CO2 and Water into Synthetic Gas
Posted: October 24, 2019 Filed under: Non-Toxic Choices Leave a commentCambridge’s artificial leaf uses two perovskite light absorbers and a cobalt catalyst to convert sunlight, water and carbon dioxide into syngas
by Virgil Andrei
The humble leaf is an incredible little machine, converting sunlight and carbon dioxide into energy for a plant. Artificial versions could be useful renewable energy sources, or even used to produce fuels. Now, researchers from the University of Cambridge have developed an artificial leaf that can produce synthetic gas (or syngas) without releasing carbon dioxide.
Syngas is made from hydrogen and carbon monoxide, sometimes with a bit of carbon dioxide thrown in. While it can technically be burned to generate electricity or for gas lighting and heating, it more often acts as an intermediate step in manufacturing products, including plastics, fertilizers, and fuels like diesel. Unfortunately, producing it can release carbon dioxide into the atmosphere.
“You may not have heard of syngas itself but every day, you consume products that were created using it,” says Erwin Reisner, senior author of the study. “Being able to produce it sustainably would be a critical step in closing the global carbon cycle and establishing a sustainable chemical and fuel industry.”
To help with that, the Cambridge team developed a new artificial leaf prototype that can produce syngas through photosynthesis. The new device contains two light absorbers made of perovskite, and a cobalt catalyst. When these are placed in water, one side produces oxygen, while the other reduces carbon dioxide and water into carbon monoxide and hydrogen. Those latter two gases can then be combined into syngas.
The team showed that the technology can still work even in relatively low light, like that on cloudy or rainy days. The perovskite was chosen because it’s good at absorbing light and creating a voltage, which is why it’s showing up in solar panels so much lately. Meanwhile the cobalt in the catalyst is lower cost and more efficient at creating carbon monoxide than other materials.
That said, the conversion efficiencies are still quite low – the new design currently produces hydrogen at an efficiency of 0.06 percent and carbon monoxide at 0.02 percent.
The new device joins a range of artificial leaf designs that are being developed to create a range of useful products, like electricity, drugs, fertilizers, and hydrogen fuel. Ultimately, the team hopes to be able to skip the middleman syngas stage.
“What we’d like to do next, instead of first making syngas and then converting it into liquid fuel, is to make the liquid fuel in one step from carbon dioxide and water,” says Reisner. “There is a major demand for liquid fuels to power heavy transport, shipping and aviation sustainably.”
The research was published in the journal Nature Materials.
Source: University of Cambridge
Scientists FINALLY Issue Warning Against Canola Oil: it Damages Your Brain, Can CAUSE Dementia, and Weight Gain
Posted: September 19, 2019 Filed under: Food and it's Impact on Our Health, Non-Toxic Choices 3 CommentsNote From Millie– I have been teaching my clients for 20 years to NOT cook with oils, any oils. Oils cannot withstand heat, it renders them highly toxic, they become rancid when separated from the foods they came from, quickly oxidizing and making them carcinogenic. They become sticky when heated, then in turn causes clogged arteries. Cook with ghee primarily because of it’s depth of nutrients, use grass fed because that cow has been in the sun long enough to store Vitamin D! Oils are good for flavoring, salad dressing, pesto, dishes that will not be exposed to heat. Buy organic, buy from oil manufactured in the US and keep it refrigerated.
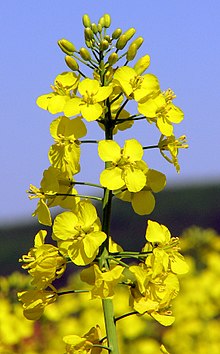 Rapeseed Plant
Rapeseed Plant
Have you ever heard of a Canola seed? You’ve probably heard of Olive and coconut trees, but not Canola right? That’s because it doesn’t exist. Canola oil is not natural oil but the commercial name of a genetically modified version of Rapeseed (which is toxic). So, it is really curious why so many “natural” food stores, even famous ones such as Whole Food’s, consistently use Canola oil in their prepared meals and Food bars (such as in their baked goods, salads, dressings, etc.)?
Canola oil was created in a Canadian university lab by Dr. Baldur Steffanson. Dr. Steffanson, after getting his newly created version of Rapeseed to meet FDA guidelines (with less toxic eurcic acid) he went on to work for Calgene (which later was acquired by Monsanto). For this reason, there is no such thing as “organic” Canola oil as the raw ingredient itself is genetically modified rapeseed.
SO WHAT ARE THE BIGGEST HEALTH RISKS OF CONSUMING FOODS THAT CONTAIN CANOLA OIL? LET’S LOOK AT A FEW:
- Canola depletes vitamin E.
- Canola increases the rigidity of membranes, which can trigger degenerative diseases.
- Because of canola’s high sulfur content, it goes rancid easily, which can exacerbate allergies and compound problems for people with bronchial or asthmatic issues.
- Human studies reveal canola causes an increase in lung cancers.
- Canola can shorten lifespan of animals and lower platelet count.
- Daily canola consumption can raise your triglycerides over 40 percent.
- Canola oil molds quickly and also inhibits enzyme function.
- It opens the door for free radicals, undermining natural antioxidants, and can be linked to increased incidence of many diseases.
- Canola leaves no foul taste when it’s spoiled, so it’s hard to tell if you’re eating rancid erucic acid.
The next time you visit the Whole Foods, or other grocers, Food court, be careful of being fooled into thinking they are the healthiest option in town. Look for all natural deli’s and food providers that use natural oils (you know the type that come from an actual plant). Most importantly remember, there is no such thing as GMO-free Canola oil.









