Alzheimer’s Risk May be 75% Higher for People Who Eat Trans Fats
Posted: October 24, 2019 Filed under: Food and it's Impact on Our Health 10 CommentsIf you eat out often, eat fast foods, eat purchased baked goods, if you eat anything with partially hydrogenated oils, canned frosting, margarines you are eating trans fats. I have worked in many high end restaurants and I can tell you that most restaurants do not use real butter, they use an oil blend, because of the cost. And those are vegetable oils that mostly contain soy, canola and other vegetable oils. Many products, such as popcorn or pizza still contain trans fat.
People with higher levels of trans fats in their blood may be 50% to 75% more likely to develop Alzheimer’s disease or dementia from any cause, according to a new study published Wednesday in the journal Neurology.
“This study demonstrates that there are negative ‘brain/cognitive’ outcomes, in addition to the known cardiovascular outcomes, that are related to a diet that has (a) high content of trans fats,” said neurologist Dr. Neelum T. Aggarwal, who was not involved in the study. Aggarwal, a member of the American Academy of Neurology, is co-leader of the Rush Alzheimer’s Disease Center in Chicago.
Over 1,600 Japanese men and women without dementia were followed over a 10-year period. A blood test for trans fat levels was done at the start of the study and their diets were analyzed.
Researchers then adjusted for other factors that could affect the risk of dementia, such as high blood pressure, diabetes and smoking. They found that people with the two highest levels of trans fats were 52% and 74% more likely to develop dementia than those with the lowest levels.
“The study used blood marker levels of trans fats, rather than more traditionally used dietary questionnaires, which increases the scientific validity of the results,” said neurologist Dr. Richard Isaacson, director of the Alzheimer’s Prevention Clinic at Weill Cornell Medicine in New York.
“This study is important as it builds upon prior evidence that dietary intake of trans fats can increase risk of Alzheimer’s dementia,” said Isaacson, who was also not involved in the study.
Trans fats can occur naturally in small amounts in certain meat and dairy foods, but by far the greatest exposure comes from the man-made version.
Also called trans fatty acids, artificial trans fats are created by an industrialized process that adds hydrogen to liquid vegetable oils to make them more solid (think of semi-soft margarine and shortening).
The food industry loves trans fats because they are cheap to produce, last a long time and give foods a great taste and texture.
Besides fried foods, trans fats are found in coffee creamer, cakes, pie crusts, frozen pizza, cookies, crackers, biscuits and dozens of other processed foods.
In the Japanese study, researchers found sweet pastries were the strongest contributor to higher trans fats levels. Margarine was next, followed by candies, caramels, croissants, non-dairy creamers, ice cream and rice crackers.
After extensive research revealed the connection between trans fats and the increase of bad cholesterol (LDL), combined with a reduction of good cholesterol (HDL), the US Food and Drug Administration banned trans fats in 2015.
Companies were given three years to stop using them; then the FDA began granting extensions to various parts of the industry. The latest extension runs out January 1.
But even if every manufacturer complies by the first of the year, that doesn’t mean trans fats are gone from the grocery shelves. According to the FDA, if one serving of the food contains less than 0.5 grams, companies can label the food as “0 grams” of trans fats.
Even in small doses, artificial trans fats will still be around to contribute to cardiovascular disease, diabetes and other conditions, such as dementia.
“In the United States, the small amounts still allowed in foods can really add up if people eat multiple servings of these foods, and trans fats are still allowed in many other countries,” said study author Dr. Toshiharu Ninomiya, a professor at Kyushu University in Fukuoka, Japan, in a statement.
“People at risk still need to pay careful attention to nutrition labels,” Isaacson said. “When it comes to nutrition labels, the fewer ingredients, the better! Focus on natural whole food, and minimize or avoid those that are highly processed.”
Aggarwal added: “This message must be delivered in countries where the ban of trans fats has not been enacted or difficult to enforce.”
Doctors Against Dairy: Cheese and Milk Linked to Breast Cancer Risk
Posted: October 20, 2019 Filed under: Food and it's Impact on Our Health Leave a comment Photo by Rebecca Orlov | Orlov Design Co on Unsplash
Photo by Rebecca Orlov | Orlov Design Co on Unsplash
In one of the more startling developments in food science, 12,000 doctors in the United States are petitioning for warning labels on cheese. “Dairy cheese contains reproductive hormones that may increase breast cancer mortality risk,” they warned.
What, is cheddar the new cigarette? No. Casein and estrogen are not nicotine and nobody’s about to blotch Brie with a label saying “Eating this kills.”
It is not suggested that eating cheese causes breast cancer. It isn’t even categorically proven that eating cheese really is associated with higher breast cancer rates, or that eating cheese causes higher mortality rates among women who already developed breast cancer. There are a lot of studies but the methodology is hardly uniform or even necessarily reliable, and there are innumerable parameters, including some that may be overriding. Like smoking, or living in nuclear waste. Those are parameters that tend to outweigh other parameters.
But the associations found so far are compelling enough for the doctors to choose to speak up.
A woman’s risk of developing breast cancer is 12.8 percent, or one in eight, in the United States. For men, it’s 0.13 percent, or just over one in a hundred.
The rate of invasive breast cancer incidence is lower, the Health Ministry told Haaretz — in Israel, it’s is 92.2 per 100,000 among Jews, and 69.8 among Arabs (compared to 124 per 100,000 in America — all figures for 2016). The older the person, the higher the probability: in Israel, almost 80 percent of breast cancer patients are aged over 50, and around 5,000 breast cancer patients are detected each year.
Certain individuals are at higher risk because of genetic factors, lifestyle factors or factors that nobody knows about yet — including, it seems, a predilection for high-fat fromage.
Among the evidence: A 2017 study funded by the National Cancer Institute that identified a 53 percent increase in the probability of breast cancer development among women who ate “the most American, cheddar, and cream cheeses.”
Another study found that among women with breast cancer, eating cheese is associated with a higher mortality risk. In a nearly 12-year follow-up, women eating one or more servings of high-fat dairy products a day (which could mean whole milk) had 49 percent higher breast cancer mortality.
“High-fat dairy products, such as cheese, are associated with an increased risk for breast cancer,” concludes the PCRM.
Proving associations between food and morbidity is extremely difficult because of the overwhelming number of parameters involved. Take cheese. What is cheese, anyway? “Dairy foods are complex mixtures which include nutrients and non-nutrient substances that could potentially influence cancer etiology, including breast cancer,” explains a separate paper published in Current Developments in Nutrition.
Let’s assume we can figure out what cheese is. If eating cheese really is associated with breast cancer, what component or components are responsible? We don’t know. If the culprit is the fat component, is there a safe level of fat in cheese? We don’t know. Does the risk outweigh the nutritional benefits of cheese to the lactose tolerant? What if the data is skewed by people lying about their cheese habit, or smoking, or diet in general, or their exposure to other carcinogens?
The culprit in cheese, if there is one, may be estrogenic hormones, though science never did understand exactly why a higher lifetime exposure to estrogen may be associated with breast cancer risk (which, again, does not mean the estrogen causes breast cancer).
Should we be eating cheese at all? Mammals wean their young, who after that turning point do not eat dairy and tend to lose their ability to produce lactase (the enzyme that digests milk and its products). But some studies do indicate that general dairy consumption — including, but not confined to high-fat — is good for us. Certainly it can be an advantage for vegetarians, if they can digest it.
In humans, the perpetuation of infantilism in the form of dairy consumption seems to have developed well after the domestication of the goat, sheep and cow some 11,000 years ago. The earliest-ever direct evidence of milk consumption was in, of all places, Britain — nowhere near where the animals were first husbanded, though whether the Neolithic farmers 6,000 years ago could actually digest the stuff or were stoic about the results of eating it is not clear.
Last year, archaeologists identified the earliest-known hard cheese, in an ancient Egyptian tomb dated to around 1615 B.C.E. It had been made of a mix of milks from sheep, goat and African buffalo.
Breast cancer, like all cancers, is enigmatic, and if there are risks they’re worth knowing about. Alcohol consumption is also associated with higher cancer risk, for instance, and yet again science isn’t sure why. Particulate smog is as well.
#mealdeliveryservice, #jax,#lactosefree,#glutenfree,#JacksonvilleFL,#nutritioncoaching, #allergies,#cancer,#energy,#higherenergy,#healing, #beyondpaleo
How Does Exercise Affect Our Microbiome?
Posted: October 18, 2019 Filed under: Food and it's Impact on Our Health Leave a comment Photo by Jacob Postuma on Unsplash
Photo by Jacob Postuma on Unsplash
So, exercise has the ability to strengthen your gut and enhance SCFA release, which is great news. But does it work both ways? Do microbes play any role in exercise performance?
A recent study would suggest that, yes, indeed they do.
Nature Medicine published the study, noting that researchers identified a specific bacterial strain called Veillonella atypica that was dramatically increased in marathon runners post-marathon. What’s cool is that this particular bacteria has the ability to break down lactic acid, which is the acid that builds up in muscles during endurance exercise. Makes sense, right?
When the scientists transferred this particular bacteria into mice, they found that the recipients had improved treadmill run time performance. Yes, they performed better athletically based purely on the presence of this microbe.
Sure, it’s an exciting finding in the world of marathon running, but what I’m most excited about is to see what we find when we study different sports. Is there a special microbe that enhances the start/stop movements in basketball or that promotes muscle recovery after a vigorous workout? My guess is the answer will be yes—but only time will tell.
Now, here’s the truth: Exercise is a good idea, regardless of whether it alters your microbiome. But that said, it’s nice to know that physical fitness also promotes gut fitness because strong guts translate into better health.
Why Dark Chocolate is Good for Your Health
Posted: October 14, 2019 Filed under: Food and it's Impact on Our Health Leave a comment
By Jesus Diaz at gizmodo.com
Confirmed: Dark chocolate is good for your heart. Really good. What’s better, scientists have discovered that people who eat 70 grams of chocolate every day increase their vascular health dramatically by “restoring flexibility to arteries and preventing white cells from sticking to the walls of blood vessels.”
The research published in the March 2014 issue of The FASEB Journal—one of the most respected publications in experimental biology—was conducted on 44 middle-aged overweight men over two periods of four weeks.
Previous investigations said that regular dark chocolate may not be that good for you because manufacturers remove flanavol from it, which is too bitter for most people. But according to Doctor Diederik Esser—one of the paper’s authors—”increasing flavanol content has no added beneficial effect on vascular health.” Adding chemical shit, however, will have an effect on your health, so please don’t stuff your faces with industrial crap chocolate sold by the likes of Hershey’s and Cadbury.
There are a lot of raw chocolate bars available, my favorite is LuLu’s
#mealdeliveryservice, #jax,#lactosefree,#glutenfree,#JacksonvilleFL,#nutritioncoaching, #allergies,#cancer,#energy,#higherenergy,#healing, #beyondpaleo
The Secret to Better Baked Potatoes? Cook Them Like the British Do
Posted: September 27, 2019 Filed under: Food and it's Impact on Our Health, In The Kitchen with Millie- How To's, Recipes Leave a commentPhoto by Monika Grabkowska on Unsplash
By Sheela Prakash thekitchn.com
If you jump across the pond to England, you’ll find baked potatoes just about everywhere, but you might not recognize them at first. That’s because they’re called jacket potatoes (which, TBH, is just about the cutest name there could be).
The difference isn’t just the name, however. The Brits take great care when it comes to their potatoes — and the results really are much crispier on the outside and fluffier on the inside than the typical American variety. A few years back, Joanna Goddard, of Cup of Jo, called out just how gloriously perfect English baked potatoes are and shared some tricks, straight from her aunt in Cornwall. Ever since trying them, my baked potato game has gotten a lot better.
Read the post: How to Make English Jacket Potatoes from Cup of Jo
Making baked potatoes isn’t difficult, but here are the tips that made the most difference.
- Slice them first. Like most Americans, I typically poke holes all over the potatoes before baking them to ensure they don’t explode in the oven. But Jo suggests slicing a cross shape about 1/4-inch thick into each potato. This helps them release some steam, makes the interior more fluffy, and also makes them easier to slice into when they’re piping hot.
- Bake them for longer than you think. Many recipes (ours included) recommend baking potatoes for an hour at 425°F. Instead, Jo suggests baking potatoes at 400°F for closer to two hours. The potatoes won’t burn at this temperature and the long bake means the skin will be so crisp that it’s practically cracker-like.
- Return them to the oven. After the two hours are up, remove the potatoes and carefully cut deeper into the slices you made initially. Then put the potatoes back in the oven for 10 more minutes. This helps to dry out the flesh further and makes it extra fluffy.
When you take those piping hot spuds out of the oven, push open that crispy, crackly, perfectly-salted skin, and drop a little butter into the lightest, fluffiest baked potato you’ve ever made, you’ll silently thank Jo and her Cornwall aunt. And you’ll know — as I now do — there’s really no other way to bake them.
Despite Growing Burden of Diet-related Disease, Medical Education Does Not Equip Students to Provide High Quality Nutritional Care to Patients
Posted: September 26, 2019 Filed under: Food and it's Impact on Our Health Leave a commentNote from Millie- Three years ago a nutrition coaching client of mine went through nursing school. During her first semester she took a class on nutrition. The proffessor was giving a talk to the many benefits of saturated fats; how crucial they are to all of the bodies processes. Read more about that- The Importance of Saturated Fats for Biological Functions. In her next semester the same professor was teaching Applied Nutrition and was teaching how bad saturated fats were for humans! So she challenged him, tried to explain what he was teaching was contradictory to what he had taught about these crucial fats being needed in the body. He became angry and pushed back. That was when she realized that she just needed to keep her mouth shut and pass the class. The medical profession is being taught very outdated nutrition information, all due to the fact that the main source of info given out to the American public by our government is derived from food lobbying, false information!
The Lancet
- Summary:
- Worldwide, nutrition is insufficiently incorporated into medical education, meaning that medical students lack the confidence, skills and knowledge to provide nutritional care to patients, according to a systematic review.
Worldwide, nutrition is insufficiently incorporated into medical education, meaning that medical students lack the confidence, skills and knowledge to provide nutritional care to patients, according to a systematic review of 24 studies published in The Lancet Planetary Health journal.
The authors recommend that nutrition education be made compulsory for all medical students, a global benchmark on the required level of nutrition knowledge for future doctors be established, and more funding be put towards developing new ways to teach nutrition in medical school.
Globally, 11 million deaths annually are attributable to poor diet, making it the leading risk factor for death across the world. Accordingly, many countries recommend that doctors apply nutrition knowledge in practice to support patients to manage lifestyle-related chronic disease and other diet-related conditions. However, these findings suggest that nutrition in medical education is lacking in all countries studied.
Author of the study, Dr Lauren Ball from Griffith University, Australia, said: “It is clear that despite the importance of nutrition for healthy lifestyles, graduating medical students are not supported with the required nutrition knowledge to be able to provide effective nutrition care to patients — a situation that has gone on for too long. Nutritional education for medical students must be improved and made a compulsory and meaningful part of the curriculum to support future doctors for the 21st century.”
To give a broad overview of nutrition education provided to medical students, the review looked at studies assessing recently graduated (ie, ?4 years) or current medical students’ nutrition knowledge, attitudes, skills, or confidence (or all three) in nutrition or nutrition counselling; the quality of nutrition curriculum initiatives for medical students; or recently graduated or current medical students’ perceptions of nutrition education.
The review included 24 studies conducted between 2012-18, including 16 quantitative, three qualitative and five studies on curriculum initiatives. The studies came from USA (11), Europe (four), the Middle East (one), Africa (one), and Australasia (seven), and the methodological quality of the studies ranged from very low to high. No published articles from Asia met the criteria for inclusion in the review.
The reviewed studies consistently found that medical students wanted to receive nutrition education to develop their skills in nutrition care but perceived that their education did not equip them to do so. Students cited both quantity and quality of their education as reasons for this — poor quality and under prioritization of nutrition in the curriculum, lack of interest and expertise in nutrition among faculty members, and few examples of nutritional counseling during clinical years to serve as models for emerging doctors.
Furthermore, students uniformly reported having a lack of required nutrition knowledge, which was also found through testing. For instance, one study found that when nutrition knowledge was assessed in a test, half of medical students scored below the pass rate.
Five studies assessing curriculum initiatives found that they had a modest positive effect. However, most nutrition initiatives were employed opportunistically as a once-off activity, rather than being integrated in a sustained way into the medical curricula. Innovative initiatives — such as online curriculum, hands on cooking experiences, and learning from other health professionals such as dietitians — showed short-term and long-term benefits for patients and health systems. Therefore, the authors call for more funding for innovative curriculum initiatives to be developed and implemented.
The authors underline that ongoing inadequate nutrition education identified in their study is likely to affect the standard of care doctors are providing to patients, not least in preventative care. Therefore, they stress the importance of institutional commitments to making nutrition education compulsory in medical training through accreditation standards and establishing benchmarks of nutritional knowledge needed by doctors before graduation.
The authors note some limitations of their study. The most frequent limitations of the studies included in the review were the absence of control groups (for the curriculum initiatives), absence of validated survey instruments to test nutritional knowledge, poor response rates, small study samples, and insufficient representativeness of the study population.
Writing in a linked commentary, Dr Stephen Devries from the Gaples Institute for Integrative Cardiology, Deerfield, Illinois, USA, notes that the beyond improving patient health, increased nutrition education could also help doctors advise on healthy diets from sustainable food systems, such as that advised by the EAT-Lancet Commission. He says: “There is much to learn about the most effective strategies to incorporate nutrition curriculum into medical training. Promising approaches to enhance nutrition education in medical education include integration of nutrition-related topics in lectures on disease pathogenesis and treatment, self-paced online curriculum, teaching kitchens, and greater utilization of interprofessional education. Identification and training of clinical mentors in nutrition is a key challenge. But what is already crystal clear, is that the worldwide state of nutrition education in medicine is inadequate. Our patients deserve much better. And so does our planet.”
Eating Garlic and Onions Daily May Drastically Cut Breast Cancer Risk
Posted: September 26, 2019 Filed under: Food and it's Impact on Our Health Leave a commentNote from Millie- Please remember that there are no foods that by themselves help us avoid cancer. It takes a daily intake that truly meets ALL of our nutrient needs to build or repair our immune system. Very few Americans come anywhere near meeting all of their needs for vitamins and minerals.
Brittany A. Roston – Sep 23, 2019, 6:18 pm CDT
Eating garlic and onions every day may drastically reduce one’s risk of developing breast cancer, according to a new study out of the University of Buffalo and the University of Puerto Rico. The researchers focused on women in Puerto Rico, where a condiment called sofrito made primarily of the two aromatics is frequently consumed.
Existing research has indicated that garlic and onions may have anti-cancer effects when consumed. The latest study looked at the potential effect of eating both of these foods instead of only one or the other. Women in Puerto Rico presented a unique opportunity for this study due to the frequent consumption of sofrito, a base sauce made with garlic and onions.
According to the researchers, the frequent consumption of this sauce means that women in Puerto Rico usually consume greater quantities of garlic and onions than women located in the US and Europe. Of note, Puerto Rico is also known for its lower rates of breast cancer compared to the rates found in the mainland states.
The study involved 314 women who had breast cancer and another 346 control subjects. After crunching the numbers, the study found that women who consumed sofrito more than one time daily had a huge 67-percent decrease in their odds of developing breast cancer compared to women who didn’t consume it as often.
The researchers found that the total amount of garlic and onions consumed daily was associated with the decreased risk, including these aromatics used in other dishes. The study points to a number of beneficial compounds found in garlic and onions that may drive the benefit, including organosulfur and flavonols.
5 Fruits and Veggies That Are More Hydrating Than Water
Posted: September 26, 2019 Filed under: Food and it's Impact on Our Health Leave a commentNote from Millie- about 15 years ago I started working with athletes who were racing in long distance races. I was also living at the beach and doing a lot of bike riding. What I finally realized was that we were all trying to hydrate, beginning 24 hours before a race or long ride and that all that was happening was that we were having to make a lot of pit stops. When we began hydrating with fruits and smoothies, performance improved drastically, we had to stop less, and didn’t get dehydrated. The body uses fruits and vegetables more effectively at hydration than it does when we drink water. We are not natural water- lappers and are meant to get most of our moisture from t he foods we eat. Now, that being said, on a Standard American Diet (SAD), that includes grains, too much protein and processed foods…you need more water to flush out the body because those foods dehydrate you.
Not a big water drinker?
You’re in luck—studies show that eating some fruits and vegetables can hydrate the body twice as well compared to drinking a glass of water. Turns out that the electrolytes, nutrients, and minerals in produce help the body retain and utilize water—kind of like drinking a sports drink or coconut water.
Keep on scrolling to learn about the most hydrating fruits and veggies you should be keep in your fridge this summer.
Cauliflower
 Photo by Irene Kredenets on Unsplash
Photo by Irene Kredenets on Unsplash
Cauliflower used to broccoli’s weird, pale cousin. Now, the low-carb veggie has become the healthy foodie’s favorite ingredient—add it in frozen to a smoothie to add density, or dice it and blend with an egg to make gluten-free “pizza dough.” It has such a mild taste, so it’s easily camouflaged by stronger flavors. But cauliflower is a nutrient-dense cruciferous vegetable that contains a surprising amount of H2O. Try adding 1 cup a day into your diet to pump up the hydration.
Watermelon
 Photo by Floh Maier on Unsplash
Photo by Floh Maier on Unsplash
I mean, c’mon, it’s in the name! Watermelon is nearly 92 percent water, and contains electrolytes like calcium, magnesium, potassium and sodium. Juicy, sweet, and oh-so-hydrating, watermelon is loaded with antioxidants like vitamin C, beta-carotene, and lycopene.
Grapefruit
 Photo by Israel Egío on Unsplash
Photo by Israel Egío on Unsplash
Bitter, slightly sweet grapefruit is a perfect choice for a summer bite if you’re following an Ayurvedic dosha diet. (Cool that internal fire, Pitta people!) Because it contains so much water and fiber, nourishing grapefruit makes for a great low-calorie snack in between meals.
Cucumber
 Photo by Ananth Pai on Unsplash
Photo by Ananth Pai on Unsplash
Chilled cucumber water is the ultimate thirst-quencher—the fresh, green taste combined with the anti-inflammatory compound caffeic acid that’s found in cukes help sooth and hydrate from the inside out.
Strawberries
 Photo by Danielle MacInnes on Unsplash
Photo by Danielle MacInnes on Unsplash
Juicy red strawberries are emblematic of the height of summer—they’re everywhere! Baked into pies, muddled into lemonade, or fresh off the vine, they’re always a welcome sight at the dinner table. At nearly 92 percent water, they’re also incredibly hydrating and contain a plethora of antioxidants that are excellent for your skin! No guilt about going overboard on the ruby berries here.
Source-
https://sporteluxe.com/us/5-fruits-veggies-hydrating-water/
Scientists FINALLY Issue Warning Against Canola Oil: it Damages Your Brain, Can CAUSE Dementia, and Weight Gain
Posted: September 19, 2019 Filed under: Food and it's Impact on Our Health, Non-Toxic Choices 3 CommentsNote From Millie– I have been teaching my clients for 20 years to NOT cook with oils, any oils. Oils cannot withstand heat, it renders them highly toxic, they become rancid when separated from the foods they came from, quickly oxidizing and making them carcinogenic. They become sticky when heated, then in turn causes clogged arteries. Cook with ghee primarily because of it’s depth of nutrients, use grass fed because that cow has been in the sun long enough to store Vitamin D! Oils are good for flavoring, salad dressing, pesto, dishes that will not be exposed to heat. Buy organic, buy from oil manufactured in the US and keep it refrigerated.
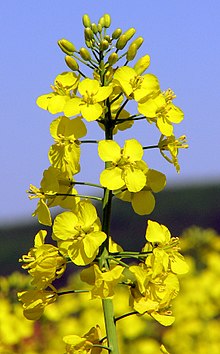 Rapeseed Plant
Rapeseed Plant
Have you ever heard of a Canola seed? You’ve probably heard of Olive and coconut trees, but not Canola right? That’s because it doesn’t exist. Canola oil is not natural oil but the commercial name of a genetically modified version of Rapeseed (which is toxic). So, it is really curious why so many “natural” food stores, even famous ones such as Whole Food’s, consistently use Canola oil in their prepared meals and Food bars (such as in their baked goods, salads, dressings, etc.)?
Canola oil was created in a Canadian university lab by Dr. Baldur Steffanson. Dr. Steffanson, after getting his newly created version of Rapeseed to meet FDA guidelines (with less toxic eurcic acid) he went on to work for Calgene (which later was acquired by Monsanto). For this reason, there is no such thing as “organic” Canola oil as the raw ingredient itself is genetically modified rapeseed.
SO WHAT ARE THE BIGGEST HEALTH RISKS OF CONSUMING FOODS THAT CONTAIN CANOLA OIL? LET’S LOOK AT A FEW:
- Canola depletes vitamin E.
- Canola increases the rigidity of membranes, which can trigger degenerative diseases.
- Because of canola’s high sulfur content, it goes rancid easily, which can exacerbate allergies and compound problems for people with bronchial or asthmatic issues.
- Human studies reveal canola causes an increase in lung cancers.
- Canola can shorten lifespan of animals and lower platelet count.
- Daily canola consumption can raise your triglycerides over 40 percent.
- Canola oil molds quickly and also inhibits enzyme function.
- It opens the door for free radicals, undermining natural antioxidants, and can be linked to increased incidence of many diseases.
- Canola leaves no foul taste when it’s spoiled, so it’s hard to tell if you’re eating rancid erucic acid.
The next time you visit the Whole Foods, or other grocers, Food court, be careful of being fooled into thinking they are the healthiest option in town. Look for all natural deli’s and food providers that use natural oils (you know the type that come from an actual plant). Most importantly remember, there is no such thing as GMO-free Canola oil.
Study Shows How Serotonin and a Popular Anti-depressant Affect the Gut’s Microbiota
Posted: September 12, 2019 Filed under: Food and it's Impact on Our Health Leave a commentA new study in mice led by UCLA biologists strongly suggests that serotonin and drugs that target serotonin, such as anti-depressants, can have a major effect on the gut’s microbiota—the 100 trillion or so bacteria and other microbes that live in the human body’s intestines.
Serotonin—a neurotransmitter, or chemical messenger that sends messages among cells—serves many functions in the human body, including playing a role in emotions and happiness. An estimated 90 percent of the body’s serotonin is produced in the gut, where it influences gut immunity.
The team—led by senior author Elaine Hsiao and lead author Thomas Fung, a postdoctoral fellow—identified a specific gut bacterium that can detect and transport serotonin into bacterial cells. When mice were given the antidepressant fluoxetine, or Prozac, the biologists found this reduced the transport of serotonin into their cells. This bacterium, about which little is known, is called Turicibacter sanguinis. The study is published this week in the journal Nature Microbiology.
“Our previous work showed that particular gut bacteria help the gut produce serotonin. In this study, we were interested in finding out why they might do so,” said Hsiao, UCLA assistant professor of integrative biology and physiology, and of microbiology, immunology and molecular genetics in the UCLA College; and of digestive diseases in the David Geffen School of Medicine at UCLA.
Hsiao and her research group reported in the journal Cell in 2015 that in mice, a specific mixture of bacteria, consisting mainly of Turicibacter sanguinis and Clostridia, produces molecules that signal to gut cells to increase production of serotonin. When Hsiao’s team raised mice without the bacteria, more than 50 percent of their gut serotonin was missing. The researchers then added the bacteria mixture of mainly Turicibacter and Clostridia, and their serotonin increased to a normal level.
That study got the team wondering why bacteria signal to our gut cells to make serotonin. Do microbes use serotonin, and if so, for what?
In this new study, the researchers added serotonin to the drinking water of some mice and raised others with a mutation (created by altering a specific serotonin transporter gene) that increased the levels of serotonin in their guts. After studying the microbiota of the mice, the researchers discovered that the bacteria Turicibacter and Clostridia increased significantly when there was more serotonin in the gut.
If these bacteria increase in the presence of serotonin, perhaps they have some cellular machinery to detect serotonin, the researchers speculated. Together with study co-author Lucy Forrest and her team at the National Institutes of Health’s National Institute of Neurological Disorders and Stroke, the researchers found a protein in multiple species of Turicibacter that has some structural similarity to a protein that transports serotonin in mammals. When they grew Turicibacter sanguinis in the lab, they found that the bacterium imports serotonin into the cell.
In another experiment, the researchers added the antidepressant fluoxetine, which normally blocks the mammalian serotonin transporter, to a tube containing Turicibacter sanguinis. They found the bacterium transported significantly less serotonin.
The team found that exposing Turicibacter sanguinis to serotonin or fluoxetine influenced how well the bacterium could thrive in the gastrointestinal tract. In the presence of serotonin, the bacterium grew to high levels in mice, but when exposed to fluoxetine, the bacterium grew to only low levels in mice.
“Previous studies from our lab and others showed that specific bacteria promote serotonin levels in the gut,” Fung said. “Our new study tells us that certain gut bacteria can respond to serotonin and drugs that influence serotonin, like anti-depressants. This is a unique form of communication between bacteria and our own cells through molecules traditionally recognized as neurotransmitters.”
The team’s research on Turicibacter aligns with a growing number of studies reporting that anti-depressants can alter the gut microbiota. “For the future,” Hsiao said, “we want to learn whether microbial interactions with antidepressants have consequences for health and disease.” Hsiao wrote a blog post for the journal about the new research.
More information: Thomas C. Fung et al. Intestinal serotonin and fluoxetine exposure modulate bacterial colonization in the gut, Nature Microbiology (2019). DOI: 10.1038/s41564-019-0540-4







